By Johanna Goldberg, Information Services Librarian
“It is difficult to imagine a slavery more senseless, cruel, or far-reaching in its injurious consequences than that imposed by fashion on civilized womanhood during the past generation. Her health has been sacrificed, and in countless instances her life has paid the penalty; while posterity has been dwarfed, maimed, and enervated, and in body, mind, and soul deformed at its behests. … [T]he tight lacing required by the wasp waists has produced generations of invalids and bequeathed to posterity suffering that will not vanish for many decades. By it, as has been pointed out by the authorities cited, every vital organ in the body has been seriously affected.”1

The title page of “Fashion’s Slaves,” 1892. Click to enlarge.
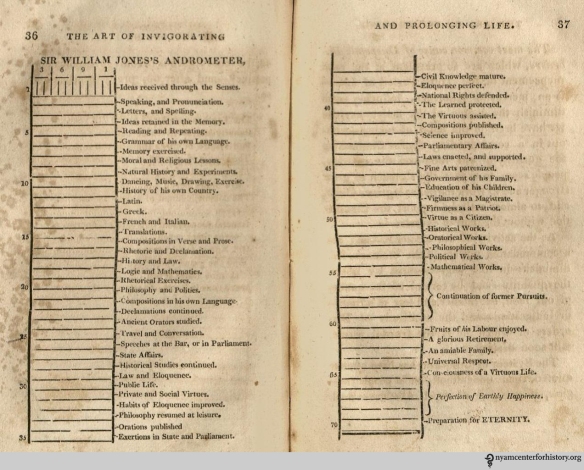
So writes Benjamin Orange Flower in “Fashion’s Slaves,” a 32-page pamphlet published in 1892 as an appeal for women’s dress reform. One of the many causes Flower takes up is the corset, expressing his concern that the undergarment causes damage to internal organs. He continues, “If women will continue this destructive habit, the race must inevitably deteriorate.”1
Certainly, many women felt fettered by their restrictive clothing or there would never have been a dress reform movement. But just how damaging were corsets?
Not all corsets were alike. Tight lacing—cinching a corset to achieve a very small, or wasp, waist—began in the 1820s and 1830s after the advent of corsets made with metal eyelets. Medical professionals came out strongly against the practice.2 As shown in dramatic X-ray images in Ludovic O’Followell’s Le Corset, tightly laced corsets could change the shape of the rib cage,3 but there is no evidence that women had lower ribs removed to decrease their waists.4
Click on an image to view the gallery from Le Corset.




By measuring 19th-century corsets and dresses, historians have determined that women probably did not cinch their waists below 20 inches.4 (By comparison, today many U.S. stores list their XXS waist size at 23.5 inches.5,6) While many waists were still quite small, they may never have gone to the 14-inch extremes reported in women’s magazines, regardless of what fashion drawings depicted.4
A tightly laced corset could reduce lung capacity, irritate skin, and weaken back and chest muscles used to being supported.2 Whether tight lacing caused long-term health issues, like reduced pelvis size, constipation and digestive issues, and reproductive problems ranging from miscarriage to uterine prolapse, is more difficult to assess and remains unclear.2,4,7

Dr. Warner trade card, inside and out. An 1883 article from Godey’s Lady’s Book and Magazine hailed Dr. Warner’s Coraline Corset as a model of comfort, superior to whalebone and horn corsets, and endorsed the model as a substitute for tight-laced models: “They have demonstrated that tight lacing is not essential to grace or beauty of form; and while impractical dress reformers have been preaching reforms which no one would adopt, Warner Brothers, by introducing properly fitting corsets, have given practical aid to the health and comfort of several million ladies.”8 Click to enlarge.
Many health problems once blamed on the corset are now clearly not the fault of the undergarment. Death caused by postpartum infections, or childbed fever, became relatively rare with the advent and spread of antiseptic techniques. With the discovery of the tubercle bacillus in 1882, it became clear that corsets did not cause the disease. Incidence of breast cancer did not decrease after corsets that did not compress the breasts came into vogue. As Gerhart S. Schwartz wrote in a 1979 Bulletin of the New York Academy of Medicine article, “one disease after another found an explanation which was unrelated to the corset.”9
Many of the doctors against tight lacing, including O’Followell, did not condemn corsets as a whole. Instead, they championed designs less tightly laced. Several pamphlets in our collection feature what they claim to be medically sound corsets.
In one, “La Grecque Corset as an Aid to the Physician and Surgeon,” printed circa 1911, the van Orden Corset Company advertises corsets that pull in the abdomen while reducing strain on abdominal muscles.10

Incorrect and correct pressure applied by corsets. In van Orden Corset Company, “La Grecque Corset as an Aid to the Physician and Surgeon,” circa 1911. Click to enlarge.
The pamphlet also features a maternity corset, “designed for a natural change of figure.”10 Corsets for maternity came on the market in the 1830s, and were often tightly laced.11 Yet the medical literature of the period does not discuss dangers of maternity corsets to the fetus or the mother,11 either due to taboos of the time or because negative impacts were rare or unreported. The maternity corset advertised by the van Orden Corset Company, from the early 1900s, was not tightly laced, taking advantage of new elasticized fabrics to expand as needed.10

La Grecque Maternity Corset. In van Orden Corset Company, “La Grecque Corset as an Aid to the Physician and Surgeon,” circa 1911. Click to enlarge.
“Corsets from a Surgical Standpoint,” from H. W. Gossard and Company (still in business today as a lingerie company), describes to physicians the benefits of prescribing their pliable front-laced corsets. These corsets, they claimed, improved posture and “preserve[d] the lines demanded by fashion, but without discomfort or injury.”12

Figures 5 and 6 in H. W. Gossard and Company, “Corsets from a Surgical Standpoint,” 1909. Click to enlarge.
Both of these pamphlets were published at the end of an era. The advent of elasticized fabric paved the way for the creation of an early bra, displayed by Herminie Cadolle at the Exposition Universelle in 1889.13 The corset’s final death knell was World War I. Women could not work in factories or the field while wearing restrictive clothing. Once household staff went to work for the war effort, upper-class women had no one to help them dress. Girdles and bras took over the corset’s supporting role, about 20 years after Flower’s calls for the end of the “destructive habit” of corsetry.1,13
References
1. Flower BO. Fashion’s slaves. Boston: Arena Pub. Co.; 1892.
2. Starr M. Vintage X-rays reveal the hidden effects of corsets. CNET. 2015. Available at: http://www.cnet.com/au/news/vintage-x-rays-reveal-the-hidden-effects-of-corsets. Accessed May 14, 2015.
3. O’Followell L. Le corset; histoire, médecine, hygiène. volume 2. Paris: Maloine; 1908.
4. Davis L. No, corsets did not destroy the health of Victorian women. io9. 2014. Available at: http://io9.com/no-corsets-did-not-destroy-the-health-of-victorian-wom-1545644060. Accessed May 14, 2015.
5. LOFT: Size Chart. Available at: http://www.anntaylor.com/catalog/sizeChartPopup.jsp. Accessed May 18, 2015.
6. Gap – women’s size chart. Available at: http://www.gap.com/browse/sizeChart.do?cid=2081. Accessed May 18, 2015.
7. Klingerman KM. Binding femininity: An examination of the effects of tightlacing on the female pelvis. 2006. Available at: http://etd.lsu.edu/docs/available/etd-04072006-115441/unrestricted/Klingerman_thesis.pdf. Accessed May 14, 2015.
8. Coraline: Its discovery and use in the manufacture of corsets. Godey’s Lady’s B Mag. 1883:468–469. Available at: https://books.google.com/books?id=nXA-AQAAMAAJ&pgis=1. Accessed May 18, 2015.
9. Schwarz GS. Society, physicians, and the corset. Bull N Y Acad Med. 1979;55(6):551–90. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1807654. Accessed May 14, 2015.
10. La Grecque corset as an aid to the physician and surgeon. New York: van Orden Corset Co.; 1911?
11. Summers L. Bound to please: A history of the Victorian corset. Oxford, New York: Berg; 2001.
12. Corsets from a surgical viewpoint. Chicago: Gossard Co.; 1909.
13. Fontanel B. Support and seduction: The history of corsets and bras. New York: Abrams; 1997.