By Paul Theerman, Associate Director, Library and Center for the History of Medicine and Public Health
“In mid-nineteenth-century America it was well understood that, aside from an occasional emergency, none but the truly indigent would voluntarily enter a hospital . . . . By the First World War all this had changed. Respectable Americans were beginning to find their way into hospitals—especially, but not exclusively, for surgery. . . . The hospital was being integrated into medical care as it already had been into medical education and the structuring of elite careers. Hospital budgets, physicians’ practice patterns, attitudes towards science, charity, and the prerogatives of class . . . interacted to transform the early twentieth-century hospital.”1
These factors—budgets, physicians, science, charity, and class—are all themes of The Knick, which focuses first on the hospital as a backdrop, then as an institution, and finally as a building. Part of the narrative arc in season two is the decision to build a new Knickerbocker Hospital uptown. This fictional plot point is in line with historical developments at the turn of the century.
For example, in the first decade of the 20th century, the new Mount Sinai Hospital could stand in for the uptown Knickerbocker. Founded in 1852 in west Midtown, Mount Sinai Hospital moved in 1872 to the East 60s, and then to its current location on Fifth Avenue at 100th Street in 1904, on the Upper East Side abutting Harlem. The city’s population moved north, and the hospital moved to follow the people, taking advantage of new buildings to advance hospital architecture generally. Under the guidance of one of America’s premier hospital administrators and builders, Dr. S. S. Goldwater, Mount Sinai developed state-of-the-art buildings to support modern, advanced medical care.2

Postcard showing Mount Sinai Hospital, 1910.
Mount Sinai Hospital is only one example of a great wave of hospital building at the turn of the century, not only in the United States, but also in Western Europe. The change can be seen through books and journal articles promoting and hoping to guide the process. At one end of the scale in hospital building was Alfred Worcester’s Small Hospitals: Establishment and Maintenance (1894, 1905, 1909), which included Suggestions for Hospital Architecture, with Plans for a Small Hospital, by William Atkinson. Worcester had no compunction about calling this “The New Hospital Movement,” and linking it to professional nursing and surgical advances. The detailed hospital plans in this book provided for an institution of about 50 beds, with possible expansion to about 75.3
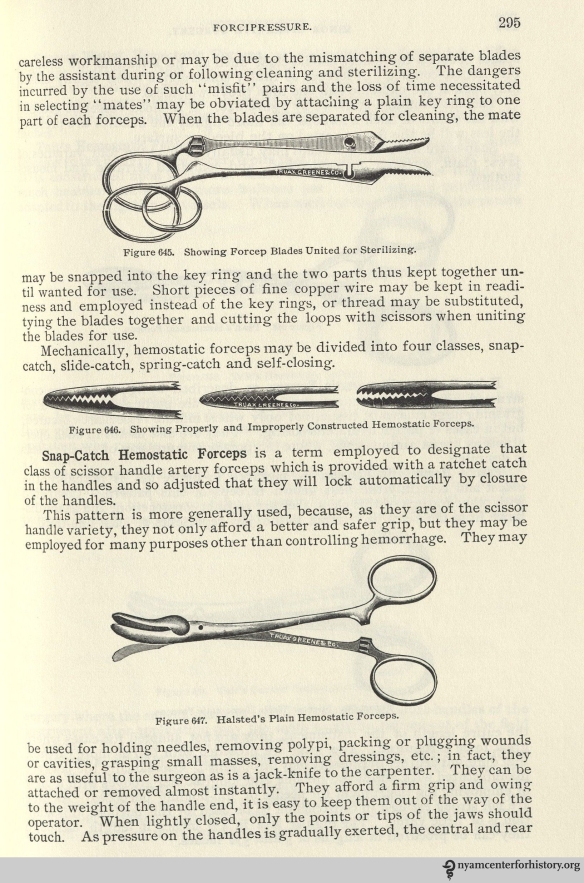
The other end of the scale can be seen in The Planning of a Modern Hospital, by Dr. Christian R. Holmes, chairman of the Board of Hospital Commissioners of Cincinnati, Ohio. In an address given at Teachers’ College of Columbia University in 1911 and published in 1917, Holmes discussed the new large urban hospital.4 He promoted the virtue of hospital architecture as a separate study and competency, giving three reasons: “Hospital construction differs from every other kind of building,” due to the ever-changing and progressive nature of medicine and sanitation, and thus requires “unusual care and foresight”; often “the men placed in charge . . . have not the slightest knowledge of the needs of a hospital”; and “the architect is often selected for reasons other than his knowledge.” Holmes supplied a typology of hospitals—pavilion, block, corridor, and composite—and then went into detail on planning a patient ward, including lighting, heating, ventilation, and bed placement and spacing, and including a room for clinical teaching.

Mount Sinai ward unit design. Figure 21 in The Planning of a Modern Hospital.
In addition to general wards, he also provided specific modifications for patients with contagious diseases; neurological conditions, including alcoholism; and venereal and dermatological diseases. He included operating theaters—a major reason for seeking a hospital at the time, and an important source of income. And he went into the specifications for all the supporting structures: kitchens, dining halls, and dormitories for staff, laundry, power plants, and of course, administration. Holmes illustrated his book with 74 photographs, elevations, and plans of large, well-known hospitals from around the United States and Western Europe. Given his background, many illustrations showed the Cincinnati General Hospital, completed in 1915, but he also included classic institutions such as the Rudolph Virchow Hospital, Berlin (completed 1906), New Royal Infirmary, Manchester (completed 1908), the Johns Hopkins Hospital, Baltimore (completed 1889), the Mount Sinai Hospital, New York (completed 1904), and Hôpital Boucicaut, Paris (completed 1897).5

Hopital Boucicaut. Figure 29 in The Planning of a Modern Hospital.
The Knick touches on issues of its time as well as of ours. The New Hospital Movement was in ascendancy more than a hundred years ago, when the show is set. But who can deny that our own time has witnessed a new hospital movement, characterized by consolidation and closures, as institutions and their buildings adapt to the new financial, social, and medical worlds of the 21st century.
References
1. Charles Rosenberg, The Care of Strangers: The Rise of America’s Hospital System (New York: Basic Books, Inc., 1987), p. 237. See also Guenter B. Risse, Mending Bodies, Saving Souls: A History of Hospitals (New York and Oxford, Oxford University Press, 1999).
2. “Two Hospitals, Two Presidents,” chapter 9 of The First Hundred Years of the Mount Sinai Hospital of the City of New York, 1852–1952, by Joseph Hirsh and Beka Doherty (New York: Random House, 1952).
3. Alfred Worcester’s Small Hospitals: Establishment and Maintenance, with William Atkinson, Suggestions for Hospital Architecture, with Plans for a Small Hospital (New York: John Wiley and Sons, 1909), pp. 1, 3, 114.
4. Christian R. Holmes, The Planning of a Modern Hospital (Detroit: The National Hospital Record Publishing Company, [1917]).
5. Holmes, The Planning of a Modern Hospital, pp. 3–13, and figures 1, 22–24, 27, and 33–74, which refer to the Cincinnati General Hospital, and figures 2, 7, 16, 21, 29, 30, and 31, which refer to the other hospitals mentioned.

![American Opium-Smokers Interior of a New York Opium Den/ Drawn by J.W. Alexander. [New York] : Harper and Brothers, Oct. 8, 1881. Courtesy of Images from the History of Medicine (NLM).](https://nyamcenterforhistory.files.wordpress.com/2014/10/exhibition-ob10382.jpg?w=584)




























![Poultney Bigelow, The Pest at Our Gates, ([New York] : Merchants’ Association of New York, [1908])](https://nyamcenterforhistory.files.wordpress.com/2014/08/pestatourgates1908_watermark.jpg?w=300&h=475)










