Today we have part one of a guest post written by Dr. Jaipreet Virdi-Dhesi, the 2016 Klemperer Fellow in the History of Medicine at the New York Academy of Medicine and a SSHRC Postdoctoral Fellow in the Department of History at Brock University in St. Catharines, Ontario. She is working on her first book, Hearing Happiness: Fakes, Fads, and Frauds in Deafness Cures, which examines the medical history of hearing loss and “quack cures” for deafness. Some of these cures are explored on her blog, From the Hands of Quacks. You can find her on twitter as @jaivirdi.
In 1935, physician Francis L. Rogers of Long Beach read a paper addressing the worrisome statistics of deafness. One study discovered nearly thirty-five thousand Americans were deaf. Another found that out of a million people tested for their hearing, 6% had significant hearing impairment. Yet another study reported three million people had some kind of hearing impairment. This “problem of deafness,” Rogers emphasized, “is primarily of public health and public welfare.” Not only were there too many people failing to adequately care for their hearing, but many cities, schools, and governments lacked the proper infrastructure to educate the public on the importance of hearing preservation. Indeed, as Rogers stressed: “Today the three great public health problems confronting the world are heart disease, cancer, and deafness.”[1]

A window display in Detroit (Hearing News, June 1942)
The notion of deafness being statistically worrying as a public health issue actually dates to the late nineteenth century, especially to the work of otologist James Kerr Love of Glasgow. Love conducted several statistical studies of the ears of deaf schoolchildren, discovering that the majority of them were not completely deaf, but had some level of “residual” hearing. With proper medical treatment, the hearing could be intensified enough to warrant a “cure.” For other cases, children could be taught to make use of that residual hearing through invasive training using acoustic aids and other kinds of hearing technologies.
Love’s research concluded that many deafness cases could actually be relieved if the ears of children were examined early and frequently—that is, deafness could be prevented. His “prevention of deafness” concept was influential for the new generation of otologists in America, especially those who were members of the New York Academy of Medicine’s Section of Otology during the first three decades of the twentieth century.
To raise awareness on the necessity of proper medical examinations and frequent hearing tests, these otologists collaborated with social organizations such as the New York League for the Hard of Hearing, which was established in 1910. The League was a progressive group catering to the needs of hard of hearing or deafened persons who were raised in a hearing society rather than in a D/deaf community and communicated primarily with speech and lip-reading rather than sign language. Composed mostly of white, middle-class, and educated members who lost their hearing from illness, injury, or progressive deafness, the League strove to construct hearing impairment as a medical issue. They argued hearing impairment was not an issue of education or communication, but rather a handicap.
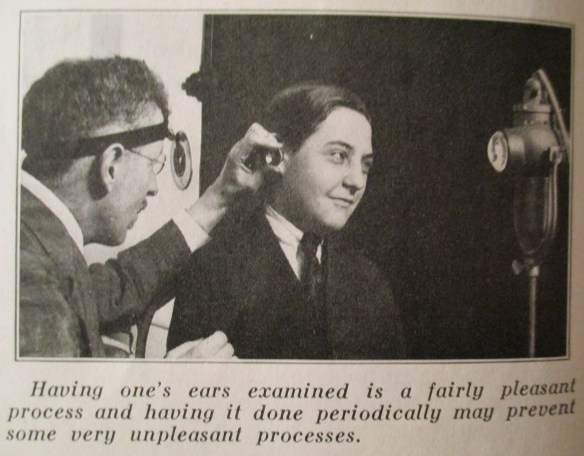
An otologist examining a young patient’s ear (Hygeia, June 1923)
The collaboration between New York otologists and the League eventually created a national network of experts, social services, teachers, physicians, and volunteers who banded together to address the so-called “problem of deafness.” That is, the problem of how to best integrate the hard of hearing, the deafened, and to some extent, even the deaf-mutes, into society. One key achievement of the League was the establishment of hearing clinics to properly assess hearing impairment, especially in children, to ensure medical care could be provided before it was too late. This project was primarily spearheaded by Harold M. Hays (1880-1940), who was recruited as president of the League in 1913, becoming the first active otologist collaborating with the League. After the First World War, Hays set up a clinic for treating hearing loss in children at the Manhattan Eye, Ear, and Throat Hospital.
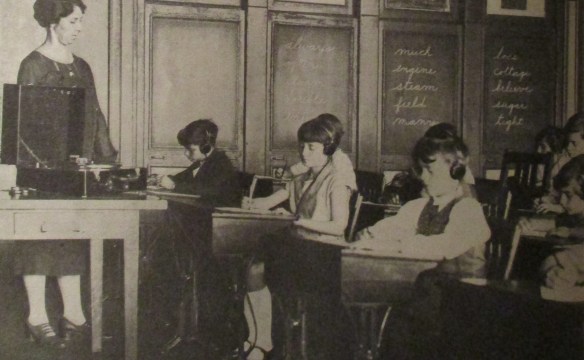
Group hearing tests of schoolchildren, using an audiometer. Headphones are used first on the right ear, then the left. (Hygeia, February 1928)
Hays claimed that hearing impairment might be a handicap, but “the sad part of it is that 90 percent of all hearing troubles could be corrected if they were treated at the proper time.” With regular hearing tests, this was possible. Yet, as Hays argued, regular hearing tests were not considered on par with other hygienic measures under public health services:
“We are saving the child’s eyes! We are saving the child’s teeth! Is it not worth while to save the child’s ears?”[2]
During the 1920s, Hays’ activism for regular hearing tests was so instrumental that in 1922, the League’s newsletter, The Chronicle, told its readers “we believe that the League would justify its existence if it did no other work than to prevent as much deafness as possible.” To achieve this mandate, the League launched a large public campaign to raise awareness on the importance of medical care. Indeed, in one report for the League, Hays remarked that with the increased publicity, there were 10,000 calls to the League in 1918 alone inquiring about aural examinations. A steady increase in patients would follow: 17 clinic patients in 1924, 326 in 1926, and then 1,531 in 1934.
Another publicity campaign spearheaded by the League was the establishment of “Better Hearing Week” in 1926, a week-long awareness program (later renamed “National Hearing Week”). Held in October, the campaign included symposium discussions on the “Problems of the Hard of Hearing,” including topics on the relationship between the physician and his deafened patient, how the deafened could build their lives, and even on newest technological developments in hearing aids. October issues of The Bulletin (the renamed League newsletter) and the Hearing News, the newsletter of the American Society for the Hard of Hearing (ASHH) included reprints of letters from prominent leaders supporting the mandates of “Better Hearing Week,” including letters from President Roosevelt and New York Mayor LaGuardia.

Advertisement for Western Electric Hearing Aid, the “Audiophone.” These before-and-after shots were powerful for demonstrating the effects of “normal” hearing, sending the message that outward signs of deafness, such as the “confused face,” could easily disappear once being fitted properly with a hearing aid. (Hearing News, December 1936)
The 1920s publicity campaigns were primarily focused on fostering ties between otologists and the League, in cooperation with hospitals and schools. In 1927, the League purchased audiometers and offered invitations to conduct hearing tests in schools across New York, so children with hearing impairment could be assessed accordingly. Two years later, the League worked with Bell Laboratories to further substantiate the conviction that deafness was a serious problem amongst schoolchildren and that something needed to be done.
At the same time otologists across America established joint ventures between organizations like the America Medical Association and the American Otological Society. They formed committees to write reports to the White House on the national importance of addressing the “prevention of deafness.” Wendell C. Phillips (1857-1934), another president of the League and the founder of ASHH, particularly emphasized the need to address the “psychologic conditions and mental reactions” of the deafened patient, for the tragedy of acquired deafness meant it is a “disability without outward signs, for the deafened person uses no crutch, no black goggles, no tapping staff.”[3] It was an invisible handicap that needed to be made visible if it was to be prevented, if not cured.
References
[1] The Federation News, August 1935.
[2] Harold M. Hays, “Do Your Ears Hear?” Hygeia (April 1925).
[3] Wendell C. Phillips, “Reminiscences of an Otologist,” Hygeia (October 1930).
































